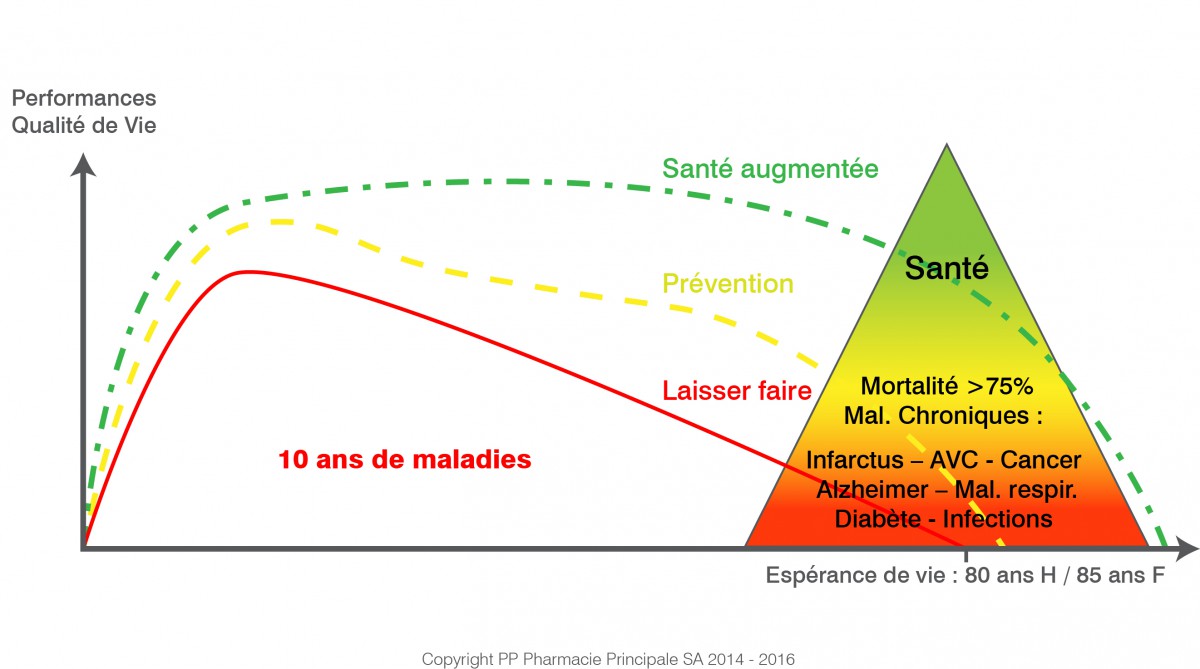
The management of chronic diseases represents a major challenge for general practitioners, who are often on the front line in the monitoring and treatment of these pathologies. These diseases, characterized by their extended duration and their gradual evolution, require a methodical and adapted approach. One of the crucial issues is the early detection, which not only reduces the severity of conditions, but also reduces the costs associated with long-term treatments. In order to effectively meet the needs of patients, it is essential to develop strategies specific, relying on tools such as the care pathway and the government action plan intended to strengthen support for chronically ill people.
|
IN BRIEF
|
There chronic disease management represents a major challenge in the field of public health. General practitioners, as the first points of contact for patients, play a crucial role in this dynamic. This article explores the different strategies that make it possible to optimize the management of chronic diseases, while taking into account the specificities of each patient.
Improved early detection
There early detection chronic diseases is essential. By identifying symptoms at an initial stage, it is possible to intervene quickly and limit the progression of the disease. Continuing training and access to adapted tools, such as care protocols, can help general practitioners strengthen their screening skills.
Personalization of care pathways
Each patient with a chronic illness has specific needs. Set up a care pathway individualized is therefore essential. This involves assessing the patient’s needs and working with other healthcare professionals to ensure effective coordination of care. The guide developed as part of the care pathway tools offers valuable recommendations for this approach.
Use of technology and management tools
Technological advances offer new perspectives for chronic disease management. For example, the implementation of surveillance systems, such as those proposed by Rock, allows regular and responsive monitoring of patients. These tools also facilitate patient education about their pathology and treatments.
Strengthening psychological support
Patient emotional well-being is inseparable from chronic disease management. Adequate psychological support can improve adherence to treatment and reduce illness-related anxiety. General practitioners must be attentive to emotional aspects and, if necessary, refer patients to specialists. Studies show that taking this aspect into account is essential to optimize health outcomes.
Multidisciplinary collaboration
There collaboration between health professionals is essential for effective management of chronic diseases. General practitioners must establish strong links with relevant specialists to ensure continuity of care. Patients will benefit from a more comprehensive approach, meeting all of their needs. The coordination of efforts between different health actors represents a major challenge in improving the quality of care.
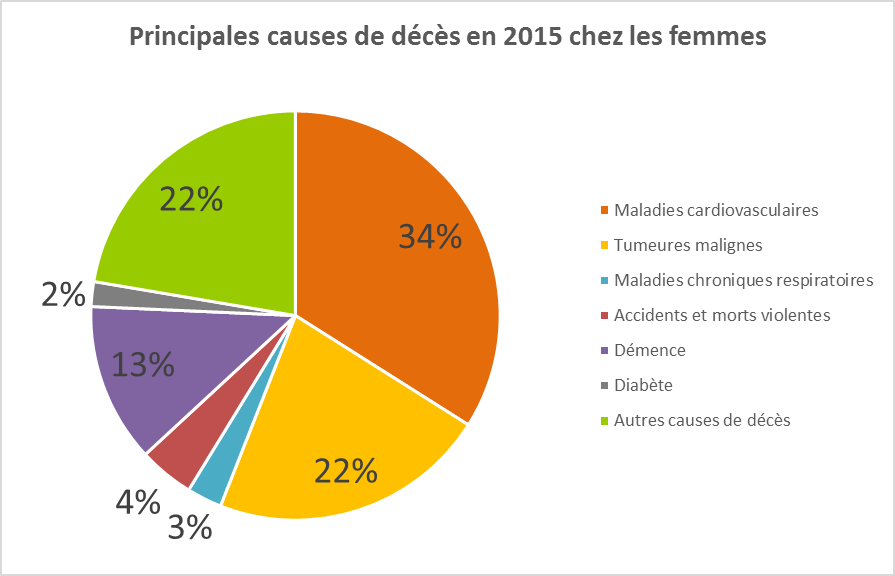
There chronic disease management is an essential component of current medical practice. Chronic pathologies, such as diabetes, hypertension, or respiratory diseases, represent a major challenge for general practitioners. Effective care requires a methodical approach, based on adapted strategies, to improve patient health outcomes while optimizing available resources. This article offers concrete recommendations for general practitioners to improve the management of chronic diseases.
Early detection and diagnosis
THE early detection chronic diseases is crucial to limit their progressive severity. Primary care physicians must implement systematic screening tools, integrating health questionnaires and regular health check-ups during consultations. Early detection not only makes it possible to effectively treat pathologies, but also to reduce long-term costs linked to serious complications. Continuing training in screening is essential for general practitioners.
Therapeutic patient education
Educating patients about their illness is essential to strengthen their autonomy and their engagement in the care process. Doctors must establish sessions oftherapeutic education, where they explain, for example, the mechanisms of the disease, the importance of compliance with treatments, as well as strategies for managing symptoms on a daily basis. By involving patients in their care journey, the effectiveness of treatments can be improved.
Care pathway planning
A care pathway well-structured is fundamental to managing chronic diseases. General practitioners must develop a personalized action plan in collaboration with the patient and other healthcare professionals. The care pathway must include regular consultations, follow-up examinations, as well as therapeutic adjustments if necessary. The establishment of an information system for monitoring actions undertaken and results observed is also recommended.
Interprofessional collaboration
There interprofessional collaboration is essential for the management of chronic diseases. General practitioners should work closely with other specialists, such as cardiologists, endocrinologists, and dietitians. Care coordination can be done through multidisciplinary consultation meetings, allowing patient data to be shared, current treatments to be examined, and recommendations adapted to each situation to be established.
Monitoring and evaluation of results
THE follow up of patients is a crucial step in the management of chronic diseases. General practitioners must put in place evaluation indicators to measure the effectiveness of treatments and the evolution of the patient’s state of health. Regular assessments, combined with discussions with patients to gather their feelings, will facilitate the necessary adjustments. The results obtained must be analyzed to identify good practices and adapt management strategies.
In a context of growth in chronic diseases, it is essential that general practitioners adopt proactive and adapted strategies to improve the care of their patients. Thanks to an integrated and structured approach, it becomes possible to optimize health outcomes while minimizing the complications associated with these pathologies.
There chronic disease management represents a major challenge for general practitioners, who are often on the front line in the monitoring and treatment of these pathologies. Chronic diseases, characterized by their longevity and scalability, require a methodical and individualized approach. Practitioners must therefore develop appropriate strategies to optimize therapeutic results and improve patients’ quality of life.
THE early detection chronic diseases is crucial. Rapid identification of conditions such as diabetes, hypertension or chronic obstructive pulmonary disease helps limit their severity and initiate early interventions. With this in mind, general practitioners must regularly raise their patients’ awareness of the importance of preventive health examinations and the detection of suggestive symptoms.
Once the pathology has been identified, the care pathway planning becomes essential. This involves creating clear protocols, developing practical guides and the use of appropriate monitoring tools. The general practitioner must strive to involve the patient in their own care, thus promoting autonomy and adherence to treatment. Communication and education about the disease are key elements in this process.
In order to improve overall care, it is also necessary to ensure interprofessional coordination. Teamwork with specialists, nurses and other health professionals makes it possible to offer holistic care, thus meeting the multiple needs of patients. By integrating these strategies, general practitioners will be able to effectively manage chronic diseases and contribute significantly to improving the healthcare system.