Interventional radiology plays an increasingly crucial role in the treatment of cancers. Thanks to technological advancements, this medical specialty significantly improves treatment methods in oncology. From the establishment of new, high-performance radiological equipment to the utilization of imaging-guided techniques, these innovations profoundly alter the landscape of cancer treatment. The increase in precision of interventions and the reduction of the invasiveness of procedures are undeniable assets for patients. This article explores the latest advancements in this field, major innovations, and the implications for the future of interventional radiology in cancer treatment.
State-of-the-art radiological equipment
One of the most remarkable aspects of medical advancements in interventional radiology is the evolution of equipment. The technology of radiology brands such as Siemens, GE Healthcare, and Philips has led to the development of more sophisticated devices that enhance treatment efficiency.
PET Scan: An advancement in diagnosis and treatment
The PET Scan (positron emission tomography) has become an essential tool in the diagnosis and treatment of cancers. The installation of a second 100% digital PET Scan at the Oncopole in Toulouse represents a significant step forward. This next-generation equipment offers increased sensitivity for detecting lesions, particularly for prostate cancer and other solid tumors. The use of innovative diagnostic tracers, such as 68Ga PSMA, allows for more precise patient follow-up and motivates the integration of targeted treatments.
Advancements in the functionality of PET Scanners allow not only for diagnosis but also for planning interventional radiology procedures, particularly due to improved visualization of tumor masses.
Cone Beam CT: A new standard for interventional radiology
Another notable innovation is the acquisition of Cone Beam CT in operating rooms. These devices enhance imaging-guided procedures during interventions. They allow for less invasive procedures, which is particularly beneficial for patients. With better access, doctors can now perform robotic punctures and other targeted interventions with unprecedented precision.
These devices also provide real-time imaging. This dynamic thus changes the approach to treatment, making interventions safer and more effective. The implementation of such technologies represents a true qualitative leap in the practice of interventional radiology.
Interventional radiology techniques in oncology
The techniques of interventional radiology are evolving rapidly. Targeted treatment procedures have gained popularity, notably due to their ability to minimize the impact on healthy tissues while optimizing the destruction of cancer cells. These methods not only reduce postoperative pain, but also improve patients’ recovery times.

Embolization: An effective targeted treatment
Among the numerous emerging techniques, embolization is a promising treatment. This technique involves injecting substances to block blood supply to a tumor, leading to its reduction or even destruction. Several studies have shown that this type of treatment is particularly effective for cancers such as liver cancer or gynecological cancers.
Treatment devices, such as LIPIOJOINT, designed by Guerbet, are making progress in this field by offering tailored embolization solutions. The designation of this product as a “Breakthrough Device” by the FDA reflects its potential. This approach also facilitates the integration of tele-imaging, thus reducing the need for travel for ongoing care.
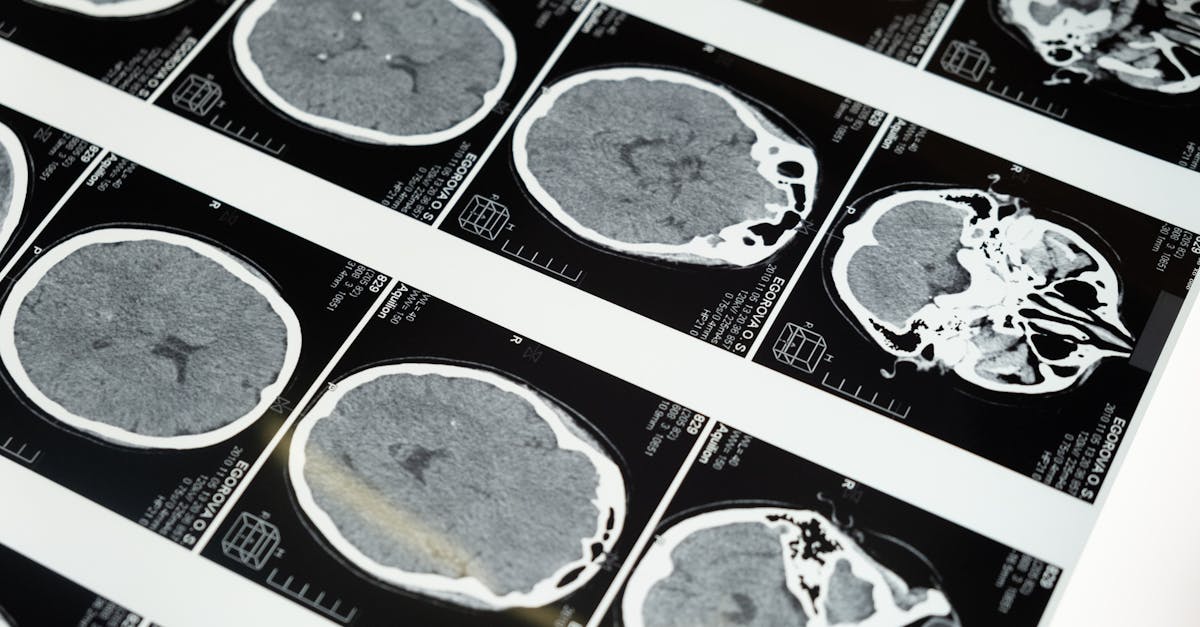
Imaging-guided techniques: Towards more precise intervention
Imaging guidance has revolutionized the way procedures are conducted. With tools like ultrasound, PET, and Cone Beam CT, practitioners can navigate with improved accuracy to reach tumors. The use of these techniques reduces the risks of complications and enhances the precision of treatments.
The ability to visualize in real time the tissue response to the intervention also allows for dynamic adjustments to treatments, thus optimizing outcomes.
The challenges and solutions in the field of interventional radiology
Despite advancements, the field of interventional radiology faces certain challenges. Understanding indications and contraindications remains a crucial topic. The guidelines for patient selection in interventional radiology must be rigorously followed to avoid postoperative complications.

Interpretation of results: A constant challenge
The safety of procedures in interventional radiology is often put to the test by erroneous interpretations of imaging results. Advances in interventional neurology highlight this need for improvement, where complex cases require innovative approaches and practical solutions. Strengthened validation protocols for results are necessary to ensure safe and effective interventions.
Specialized training: An imperative for the future
The need for continuous training in this field is pressing. Professionals must be adequately trained to use new techniques and equipment. As technologies evolve, updating skills is essential to maintaining high standards of care.
In this regard, participating in seminars and implementing practical training sessions can be beneficial for both physicians and care teams. Such efforts will contribute to ensuring the efficiency and safety of treatments in interventional radiology.
Innovations in oncology: Towards new perspectives
Finally, innovations in oncology, particularly in interventional radiology, incorporate new dimensions that transform the medical landscape. Beyond conventional techniques, the focus is on more personalized treatments, tailored to the specificities of different types of cancers and patients.
Theranostics: A new frontier
A promising development in this context is the emergence of theranostics, which combines diagnostic and personalized treatment. This approach could potentially maximize the chances of success of therapies by precisely adapting treatments according to each disease’s profile.
For example, the use of radiopharmaceuticals allows for the targeting of specific tumors while providing critical information to assess the therapeutic response.
Interdisciplinary collaboration: The future of cancer treatment
The future of treatment through interventional radiology also relies on interdisciplinary collaboration between oncologists, radiologists, and other specialists. This global partnership is essential to optimize treatment protocols and ensure integrated, high-quality care.
Study results show that these collaborative approaches often lead to better patient outcomes, both in terms of treatment response and post-therapeutic quality of life. The combination of varied expertise fosters comprehensive analysis and management of complex cases in oncology.
A promising future for patients
Innovations in interventional radiology pave the way for safer, more effective, and less invasive treatments for cancer patients. With the continuous development of technologies and treatment methods, it is reasonable to be optimistic about the future of oncological care. Practitioners are now better equipped to face the challenges posed by cancers, thus offering treatment options that can truly improve patients’ lives. The commitment to research and development in this field reflects a continuous promise of hope in the fight against cancer.
| Technique | Description | Advantages |
|---|---|---|
| PET Scan | Imaging for early detection of cancers. | Increased sensitivity, early diagnosis. |
| Embolization | Technique aimed at blocking blood flow to the tumor. | Minimizes invasiveness, effective against certain tumors. |
| Cone Beam CT | 3D imaging for precise surgical interventions. | Improved guidance, real-time. |
| Theranostics | Combining diagnostic and personalized treatment. | Precise targeting, optimized treatment. |