The management of cerebral aneurysms has significantly evolved thanks to the emergence of new interventional techniques. These approaches, combining surgery and embolization, allow for precise assessment of rupture risks and better customization of treatments. Among the innovations, the use of interventional neuroradiology and devices such as flow diverters illustrate significant advances in this field, thus reducing postoperative complications and improving success rates. The medical management of cerebral aneurysms is now oriented towards minimally invasive techniques and preservation of neurological functions.

Cerebral aneurysms, vascular anomalies located on the arteries of the brain, represent a neurological pathology of great importance. Early detection and treatment are crucial as they can lead to severe complications, notably ischemic or hemorrhagic strokes. The management of aneurysms has undergone a revolution with the development of state-of-the-art interventional techniques, allowing for less invasive and more effective approaches.
Traditionally, intracranial aneurysms were treated through open surgery, where a clip was placed to occlude the aneurysm. However, these surgical methods present complications and prolonged recovery times, hence the need to develop minimally invasive alternatives. Today, two main approaches are considered relevant: endovascular embolization and microsurgical clipping.
Embolization is a technique that involves occluding the aneurysm by introducing a catheter into the blood vessels, typically through a puncture in the femoral artery. This catheter is guided to the aneurysm using angiographic imaging. Various materials can be used for embolization, including platinum coils or more modern devices such as WEB embolization devices or flow diverters.
WEB devices, a recent innovation, allow for an intra-aneurysmal treatment that reduces blood flow within the aneurysm without occluding the parent vessel. This promotes a gradual thrombosis of the aneurysm while preserving blood flow to adjacent cerebral territories. The use of flow diverters also represents a significant advance, as these devices modify blood flow in a way that promotes natural vessel repair and decreases pressure within the aneurysm.
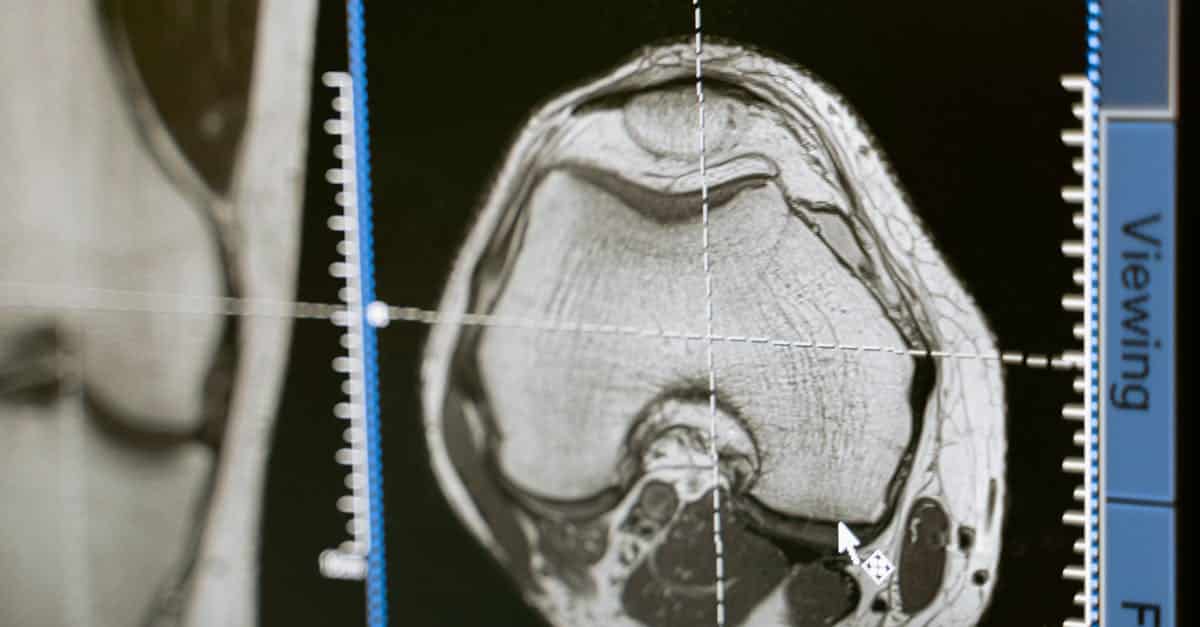
Another crucial aspect of managing cerebral aneurysms is interventional radiology. Interventional neuroradiology techniques guide treatment and allow access to aneurysms through less invasive pathways. These procedures utilize advanced imaging techniques such as MRI or CT scans to plan interventions and guide instrumentation. This reduces the risk of complications and allows for better evaluation of vascular repairs performed.
Despite these advances, preoperative assessment remains essential. A thorough examination, including brain imaging such as cerebral angiography, allows for determining the size, morphology, and precise location of the aneurysm, prerequisites for developing a personalized treatment plan. Post-interventional monitoring is also crucial to detect any potential complications, such as clots or recurrent bleeding, and to ensure the effectiveness of embolization or clipping.
The possible complications of interventional treatments include allergic reactions to contrast agents, vascular injuries during catheter insertion, or infections. Furthermore, long-term follow-up is essential. This may include regular imaging checks to ensure that the aneurysm remains occluded and to assess the health of adjacent vessels.
These advances in the treatment of cerebral aneurysms have enabled a better approach regarding the safety index and the success rates of procedures. Patients benefit from safer care, shorter hospital stays, and faster recovery. Minimally invasive approaches also pave the way for more in-depth clinical studies aimed at further evaluating their effectiveness compared to traditional surgical interventions.
In this constantly evolving medical context, it is imperative for health professionals to stay informed about the latest technological innovations and management protocols. Multidisciplinarity, involving neurologists, neurosurgeons, and neuroradiologists, proves essential for ensuring optimal management of cerebral aneurysms.
In conclusion, the new interventional techniques in the treatment of cerebral aneurysms lead to better patient management, reducing risks associated with interventions and improving clinical outcomes. This represents a paradigmatic shift in the therapeutic approach to intracranial aneurysms, thereby promoting a culture of patient-centered care and medical safety.

The management of cerebral aneurysms has significantly evolved thanks to the emergence of new interventional techniques. These minimally invasive procedures offer effective alternatives to traditional surgical methods, thereby improving the prognosis for patients at risk of aneurysm rupture. This article highlights the latest advances in this field, focusing on embolization techniques and the use of specific devices.
Embolization Techniques
Embolization represents a non-surgical approach recommended for the treatment of cerebral aneurysms. This process involves obstructing the aneurysm by injecting specific materials via an intravascular access. The most common technique is coiling, where metal coils are placed inside the aneurysm to induce thrombosis. This reduces the pressure inside the aneurysm and decreases the risk of rupture.
Another promising embolization technique is the use of the WEB (Woven EndoBridge) system. This device is designed to more effectively treat wide-necked aneurysms by allowing for tailored and personalized occlusion of the aneurysm. Its efficacy has been demonstrated in various clinical studies and could become a standard in the treatment of these vascular anomalies.
Use of Flow Diverters
Flow diverters represent a major advancement in the treatment of complex intracranial aneurysms. These devices are placed in the blood vessel carrying the aneurysm, allowing for the rerouting of blood flow while promoting clot formation within the aneurysm. This method has the advantage of preserving the integrity of vascular branches and reducing the risk of postoperative complications.
The clinical results obtained through this technique demonstrate a significant improvement in the healing rates of aneurysms, particularly for those that are not amenable to more traditional methods. However, it is essential to carefully assess each case to determine the appropriate indication for this type of treatment.
Minimally Invasive Neurosurgery
Alongside embolization techniques, minimally invasive neurosurgery has also seen considerable growth. This approach involves performing surgical interventions using specialized instruments and advanced imaging techniques, such as endoscopy. One example of these interventions is microsurgical clipping, which involves placing a clip on the neck of the aneurysm to separate it from the vascular system, thereby preventing rupture.
The combination of these traditional surgical methods with new technologies allows for a personalized treatment of aneurysms. Tools such as robotics and computer-assisted navigation enhance the precision of interventions and reduce postoperative recovery time.
Preventive Management and Follow-Up
It is crucial to adopt a preventive approach to the management of cerebral aneurysms. Advanced imaging techniques, such as MRI and CT scans, allow for the detection of asymptomatic aneurysms at early stages, providing intervention opportunities before a rupture occurs. Employing regular follow-up strategies for patients with significant risk factors (such as hypertension or family history) is also essential.
Finally, involving patients in their own follow-up and treatment is integral to improving clinical outcomes, fostering informed decisions and better adherence to therapeutic recommendations.