The prescription of prednisolone is generating increasing interest in the medical field, particularly due to its extensive use in treating inflammation and autoimmune diseases. This corticosteroid, which works by altering the body’s immune response, provides relief from a variety of symptoms, ranging from joint pain to respiratory conditions. However, its effectiveness is accompanied by numerous potential side effects that healthcare professionals must carefully evaluate before any prescription.
Patients may face undesirable consequences such as water retention, high blood pressure, or hormonal disorders. It is also essential to consider contraindications, as certain health conditions may be exacerbated by the use of prednisolone. Thus, the relationship between therapeutic benefit and the risks involved becomes a major issue. Doctors must ensure rigorous monitoring, especially in cases of prolonged treatment, in order to adjust dosages and prevent potential complications. In summary, the prescription of prednisolone requires a thorough evaluation of risks and benefits to ensure optimal patient management.
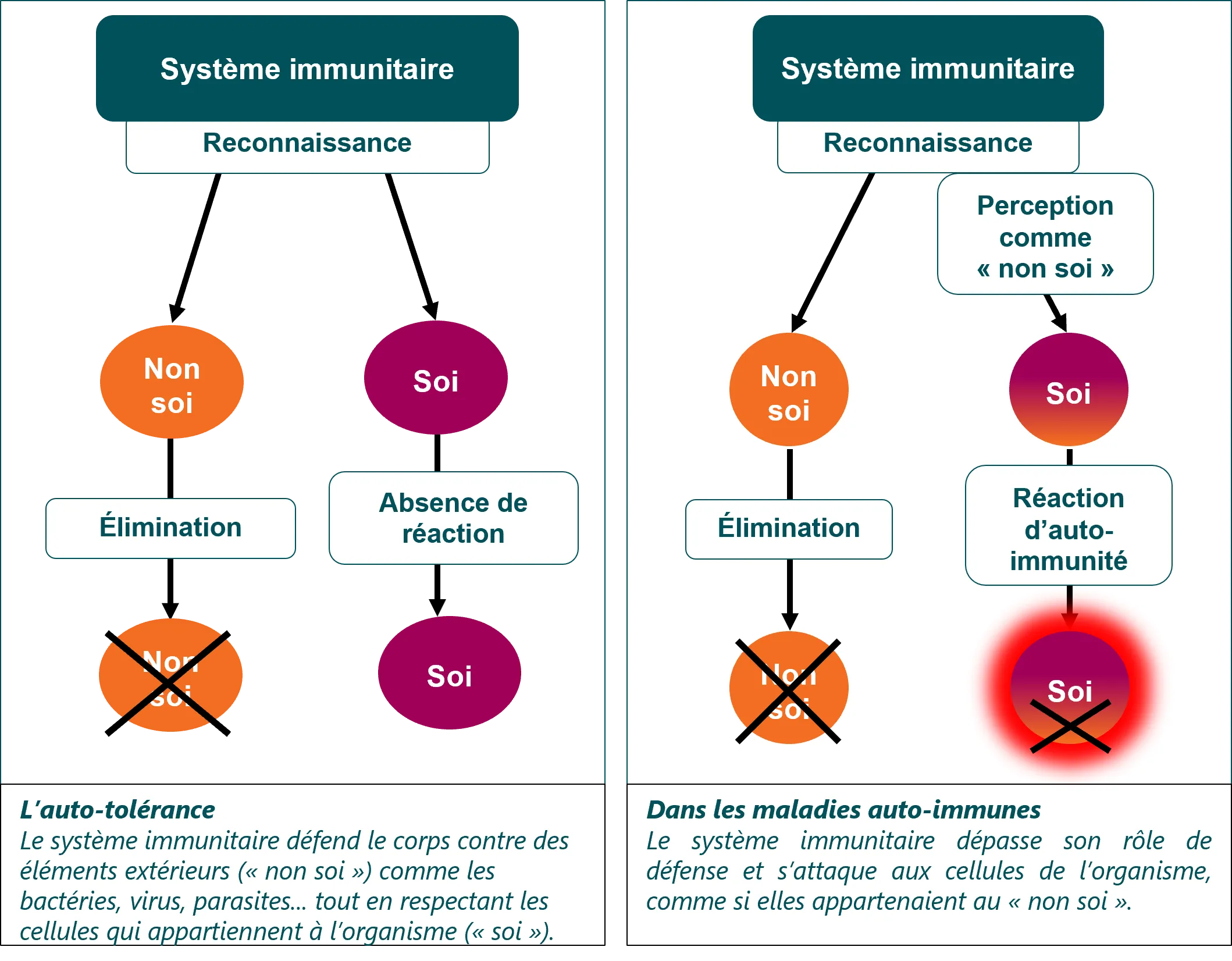
Prednisolone is a corticosteroid often prescribed for its anti-inflammatory and immunosuppressive properties. It is used in the treatment of various conditions such as autoimmune diseases, certain forms of arthritis, as well as allergic and dermatological conditions. However, despite its therapeutic benefits, prednisolone can lead to a series of undesirable effects and has contraindications that require special attention during its prescription.
Possible side effects of prednisolone
Like any medication, prednisolone is prone to cause side effects. These largely depend on the dose, duration of treatment, and the individual sensitivity of the patient. Among the most common undesirable effects, we note:
Water retention: Prednisolone may promote sodium and water retention, leading to peripheral edema. Careful monitoring of weight and hydration status is thus advised.
High blood pressure: The consumption of prednisolone can induce hypertension, particularly at high doses. Patients with pre-existing hypertension must be regularly monitored for their blood pressure.
Metabolic problems: Taking this medication can lead to an increase in appetite and weight gain, and even insulin resistance, potentially leading to the development of type 2 diabetes. Patients should be informed and monitored regarding their blood sugar levels.
Gastrointestinal disorders: Effects such as nausea, abdominal pain, or even heartburn may manifest. To reduce these disturbances, it is often advised to take the medication with food.
Infectious risks: As an immunosuppressant, prednisolone increases the risk of infections. Patients should be vigilant for any signs of infection and consult their doctor if in doubt.
Tendinopathies: The use of corticosteroids may promote the onset of tendinopathies and even, in exceptional cases, lead to tendon rupture. Patients should be informed to monitor any potential pain during joint movements.
Contraindications to the prescription of prednisolone
Prednisolone should not be administered without precautions. Certain contraindications must be taken into account before prescribing it:
Uncontrolled systemic infections: The use of this medication is contraindicated in cases of uncontrolled bacterial, viral, or fungal infections due to its immunosuppressive effect that can worsen the patient’s condition.
Gastric ulcers: The presence of gastro-duodenal ulcers constitutes a contraindication, as prednisolone may exacerbate this condition.
Uncontrolled diabetes: Diabetic patients should be closely monitored, and the prescription of prednisolone should be considered with caution. It is essential to evaluate the need for insulin or other hypoglycemic treatments in these cases.
Osteoporosis: Corticosteroids are associated with bone loss. Thus, prescription in patients suffering from osteoporosis is not recommended without adequate prevention, particularly with anti-osteoporotic treatments.
Heart disease and kidney failure: Individuals suffering from congestive heart failure or renal failure must receive rigorous medical follow-up during treatment with prednisolone. The choice of dose and duration must be meticulously evaluated.
In summary, prednisolone has a range of varied clinical applications. Nevertheless, its use must always be accompanied by a rigorous evaluation of potential side effects and contraindications to ensure patient safety. Each prescription must be individualized and include regular follow-up to adjust treatment if necessary. For further information on this medication, you can refer to the resources available on Vidal or Doctissimo, which discuss in more detail the uses and precautions related to prednisolone.
FAQ on the medical prescription of prednisolone: side effects and contraindications
What are the common side effects of prednisolone? Common undesirable effects include water retention, increased blood pressure, and hormonal disorders such as reversible diabetes.
When is it recommended to consult a doctor while taking prednisolone? It is advisable to immediately inform your doctor if you experience tendon pain or limited movement.
What are the risks associated with long-term use of corticosteroids such as prednisolone? Prolonged use can cause issues such as insulin resistance, increased appetite, and other metabolic disorders.
Is prednisolone contraindicated for certain people? Yes, its use is generally discouraged in patients with active infections, severe digestive disorders, or heart problems.
Can prednisolone cause an increase in blood pressure? Yes, one of the potential side effects of prednisolone is an increase in blood pressure.
What symptoms should be monitored during treatment with prednisolone? It is important to monitor for signs of tendinopathy, as well as sudden weight changes and sleep problems.
Can prednisolone affect blood sugar control? Yes, it can reduce glucose tolerance and promote the occurrence of drug-induced diabetes.