Robotic surgery represents a significant advancement in the medical field, offering undeniable benefits in terms of precision and post-operative recovery. However, its adoption raises questions regarding the associated costs. An analysis of these expenses requires a cost-benefit evaluation, taking into account not only the high initial investments but also the potential long-term economic gains, as well as the improvement in patient outcomes. Through a methodical approach, this topic raises challenges and opportunities, leading to a reflection on the economic sustainability and the future of this technology in surgical practices.

Robotic surgery represents a major advancement in the medical field, combining surgical precision with advanced technologies. Developed over the past two decades, it is gradually becoming established in the healthcare world, with a range of applications in oncology, urology, and other surgical specialties. However, despite its undeniable advantages, the costs associated with these technologies remain a subject of debate. In this analysis, we will examine in depth the economic dimensions of robotic surgery, considering the initial costs, potential savings, and long-term clinical benefits.
First of all, it is essential to emphasize that the costs of a robot-assisted intervention include several aspects, such as the acquisition and maintenance costs of surgical robots, the training costs for surgical teams, as well as the operational costs related to each intervention. In general, the robots used for procedures such as prostatectomy, colorectal surgery, and thoracic interventions require substantial initial investment, which can reach several million euros.
The acquisition costs can be disruptive for healthcare facilities, especially in a context where budgets are tight. The maintenance costs and the fees associated with the usage of the technology can also accumulate quickly. These elements must be taken into account when evaluating the economic viability of integrating robotic surgery into a hospital or clinic.
On the other hand, it is crucial to consider the long-term savings that may arise from the use of robotic surgery. Studies have shown that, although initial costs are high, robot-assisted interventions can lead to a reduction in hospital stays, less blood loss, and a decreased risk of complications such as incontinence. Therefore, these factors can contribute to a decrease in the overall healthcare costs in the long run.
Cost-benefit analyses conducted in various healthcare facilities have shown that robotic surgery can offer superior clinical outcomes, leading to increased patient satisfaction and thus potentially greater efficacy of care. The impact on the post-operative recovery of patients is also notable; thus, the reduction of aftereffects contributes to limiting rehabilitation costs.
A study conducted at the Rouen University Hospital illustrates the economic impact associated with the adoption of robotics in minimally invasive lung resection surgery. The costs related to the purchase of equipment and the initial training of surgeons were compared with the costs of post-operative care and follow-up recommendations. The results indicate that, although the costs of introducing the technology are considerable, the reduction of post-operative complications and the decrease in hospital stay duration have led to net financial savings in the long term.
Another fundamental aspect to consider is the training of surgeons. Robotic surgery requires specialized teaching and particular expertise. Institutions wishing to integrate this technology must invest in adequate training programs to ensure safe and efficient practice. The training aspect is essential to minimize potential errors and maximize the success of interventions, which could in turn have implications for correction costs in case of complications.
Companies that manufacture surgical robots also highlight the constant technological advancements that optimize the performance of devices. As technology progresses, there is hope that acquisition costs will decrease while efficiency improves. Surgical robotics will likely continue to evolve, offering innovative features and enhanced performance, which could justify the initial investment in the future.
Nevertheless, the issue of socio-economic challenges related to the use of robotics in surgery also merits discussion. Indeed, investment in this technology could increase disparities in access to healthcare. Less well-funded institutions may find themselves unable to acquire such systems, which could widen the gap between different healthcare structures. This is a challenge that the healthcare system must address to avoid penalizing patients and ensure equal access to quality care.
The impact of robotic surgery also varies depending on the specific procedures performed. Some studies suggest that the most complex surgical interventions may benefit more from the robot-assisted approach. For example, in oncology, operations requiring high precision can achieve significantly improved outcomes thanks to robotic devices. Thus, the return on investment could be more pronounced for highly specialized procedures compared to other relatively simple interventions.
Finally, in a context of growing economic pressure and the demand to optimize healthcare spending, robotic surgery must be accompanied by a rigorous and ongoing evaluation. Continuous monitoring of clinical and economic outcomes will help determine the effectiveness of this unique technology in various medical disciplines. It is crucial to conduct longitudinal studies to adjust economic approaches related to robotics and new technologies to avoid it becoming a prohibitive option for healthcare institutions.
In terms of patient flow management, robotic surgery could also help to alleviate certain services by allowing for faster and less invasive interventions. This could result in an optimization of hospital resource utilization, with a substantial reduction in long-term costs. Indeed, every minute saved on intervention times and any efficiency gains could lead to an improvement in results. Therefore, institutions adopting these technologies must consider passing these benefits on to their management practices.
In summary, the costs of robotic surgery must be viewed from a comprehensive economic perspective. While the initial investment may seem prohibitive, the potential savings generated by the reduction of complications and improvements in care provide a solid justification for this technology. With the ongoing development of robotic surgery and an increased focus on training and cost optimization, the balance between costs and benefits is gradually tipping. The future of this technology promises to be exciting, with an emerging position that could permanently transform the surgical landscape.

Robotic surgery, while revolutionary, raises a multitude of questions regarding its economic viability. The analysis of the costs associated with this surgical technique, as well as the benefits it can generate, proves essential to justify its adoption within healthcare institutions. This article explores various financial aspects of robotic surgery, while considering clinical and logistical implications.
Evaluation of Initial Costs
The initial investments for acquiring robotic surgery systems are considerable. This cost includes the purchase price of the robot, which can exceed several million euros, as well as the expenses related to its installation and the training of surgical teams. Furthermore, maintaining this equipment requires ongoing investments in terms of maintenance and technological updates. These elements must be carefully considered when evaluating the profitability of integrating such technology into a healthcare institution.
Impact on Hospital Stay and Recovery
One of the main advantages of robotic surgery lies in its ability to reduce the length of hospital stays for patients, compared to traditional surgical techniques. Patients undergoing robotic intervention usually demonstrate faster recoveries, which translates to shorter hospital stays and, consequently, a decrease in the costs associated with hospitalization. This reduction can compensate for the initial costs over time, making the technology more appealing in the long run.
Clinical Cost-Benefit Analysis
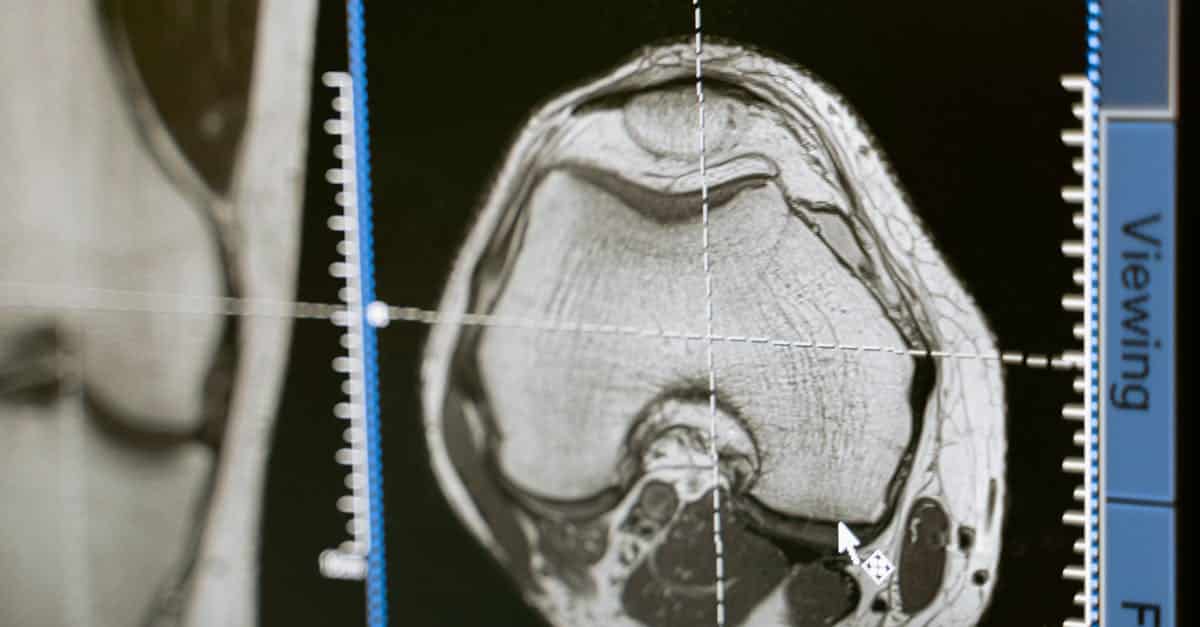
A medical-economic analysis is essential to relate the operating costs of robotics to the clinical benefits it provides. Studies show that surgical interventions performed using robotics can lead to fewer complications and improved post-operative outcomes. This is particularly relevant in areas such as urology and oncological surgery, where effective treatments are crucial for patient well-being. The established link between costs and outcomes must be emphasized in discussions regarding the relevance of integrating robotics in hospital settings.
Society and Perception of Costs
The perception of costs by society and stakeholders in the healthcare sector plays a significant role in the acceptance of robotic surgery. An increased awareness of the long-term benefits, both operationally and humanly, should be encouraged to justify the required investments. Patients and their families, when informed about the clinical benefits and the potential long-term savings, may be more inclined to support such initiatives, thus contributing to greater acceptance of medical innovations.
In the context of Robotic surgery, cost analysis cannot be limited to a linear evaluation of initial expenses but must also include an analysis of clinical outcomes and long-term savings. A deep reflection on these aspects will allow healthcare institutions to make informed decisions regarding the use of this innovative technology.